Abstract
Background: Survival outcomes in adolescents and young adults (AYA) with cancer have not improved at the same rates as those in children. Studies in AYA with acute lymphoblastic leukemia (ALL) have shown that pediatric-based treatment protocols result in better survival compared to adult protocols. Consequently, many adult centers have begun to treat AYA ALL with pediatric protocols. Whether this change in practice has diminished survival disparities between pediatric and adult centers has not been established.
Methods: The IMPACT Cohort comprises all Ontario, Canada AYA 15-21 years old diagnosed with one of six common cancers (including ALL) between 1992 and 2011. Detailed demographic, disease, treatment, and outcome data were collected through chart abstraction and validated by content experts. Locus of cancer care (pediatric vs. adult center) was determined based on where the majority of chemotherapy was delivered in the first three months after diagnosis. Linkage to population-based health administrative data identified cancer events (relapse, death) that were not detected through chart abstraction. Various predictors of locus of care were examined, including age (continuous variable), gender, time period (1992-1998 vs. 1999-2005 vs. 2006-2011), rural residence, and socioeconomic status using logistic regression. The impact of the above predictors and of locus of care on event-free (EFS) and overall survival (OS) was determined using Cox proportional hazard models. Events included disease progression, relapse, death, and second malignancies.
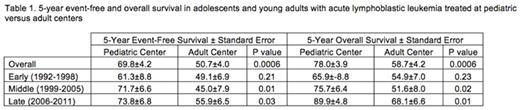
Results: The cohort included 271 patients with ALL, 152 (56%) of whom received therapy at an adult center. In multivariable analysis, older patients [odds ratio (OR) 11.9 per year; 95th confidence interval (CI) 6.1-25.0] and those in the earliest time period (1992-1998 vs. 2006-2011, OR 3.5; 95CI 1.1-10.7) were more likely to be treated in an adult center. The 5-year EFS of patients treated at a pediatric center was 69.8%±4.2% vs. 50.7%±4.0% at adult centers (p=0.0006). 5-year OS was 78.0%±3.9% vs. 58.7%±5.5% (p=0.0006). For the entire cohort, there was no significant improvement in EFS over time. In multivariable analysis, only locus of care was significantly associated with EFS [adult vs. pediatric hazard ratio (HR) 4.0; 95CI 1.4-11.9]; age and time period were not predictive. The disparity in both EFS and OS between pediatric and adult cancer centers widened over time (Table 1). In the earliest time period (1992-1998) there was no significant different in OS between adult vs. pediatric centers (HR 1.8; 95CI 0.8-4.3). The HR increased and became statistically significant in the middle time period (1999-2005; HR 2.4; 95CI 0.9-5.6) and widened further in the most recent time period (2006-2011; HR 4.3; 95CI 1.4-13.8).
Conclusions: Despite studies showing improved survival outcomes in AYA with ALL treated on pediatric-based protocols, and the increased use of such protocols at adult centers, outcomes in Ontario did not improve over the 20-year study period. Contrary to expectations, disparities in survival between pediatric and adult centers widened, with the largest disparities seen in the most recent time period. These results suggest that at a population-level, the use of pediatric protocols may not be sufficient to abolish locus of care-based outcome disparities. Future analyses will look at the impact of protocol adherence, delays in therapy, toxicity, and hospital volume on survival.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal